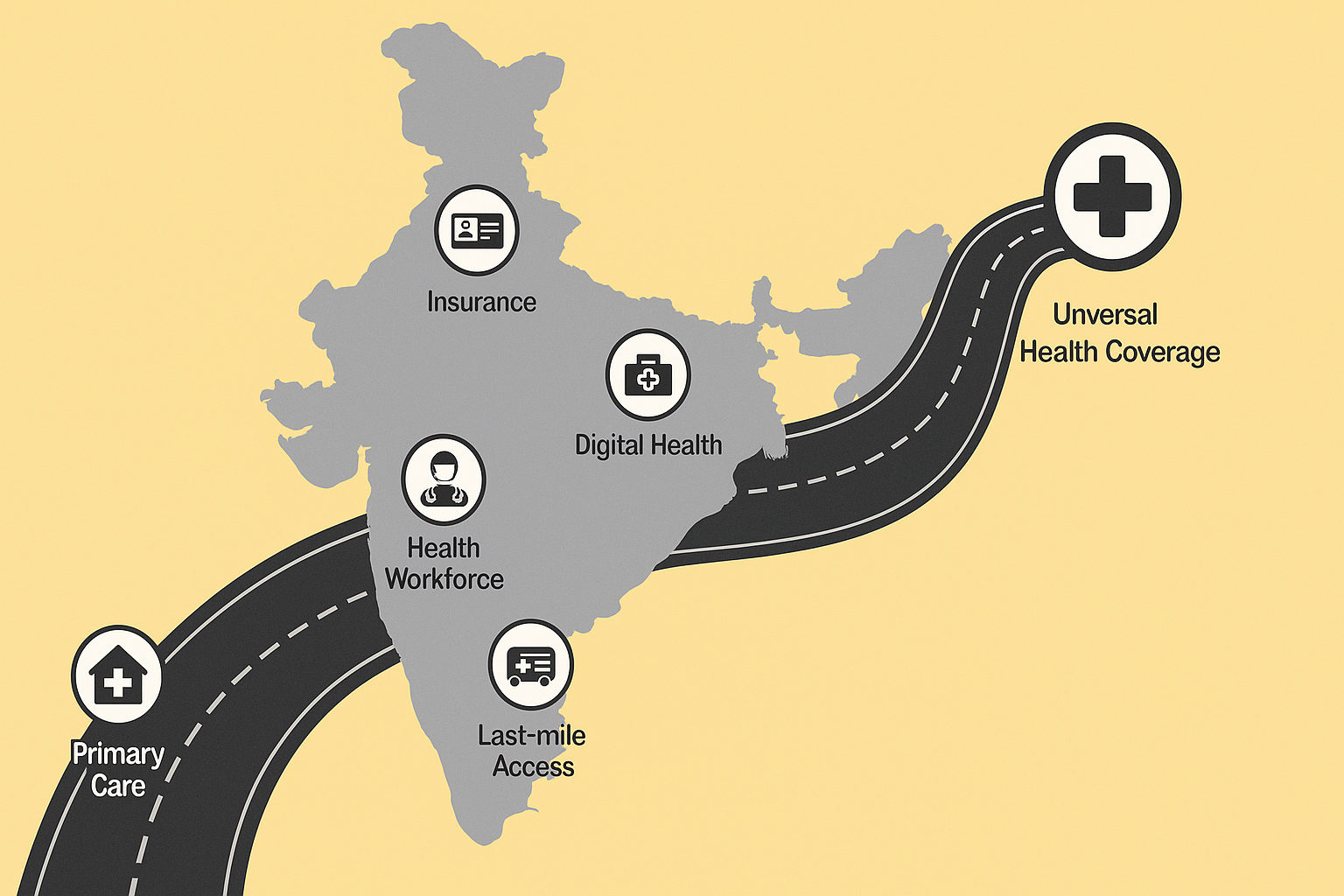
Road map for universal health coverage in India
Hindustan Times
I. AUTHOR’S CENTRAL ARGUMENT
The author argues that for India to achieve Universal Health Coverage (UHC) by 2030 and fulfil the vision of Viksit Bharat 2047, its health system must be agile, adaptive, and anticipatory. This means strengthening primary healthcare, ensuring assured service delivery, promoting prevention and health promotion, building resilient systems, and addressing inequities, gender gaps, and the rising burden of non-communicable diseases.
The central thesis is that UHC is achievable only through coordinated reforms across service delivery, workforce preparedness, financing mechanisms, and community engagement, supported by a strong public health foundation.
II. KEY ARGUMENTS PRESENTED
- India Must Deliver on UHC Commitments by 2030
– The government must assure essential services at all levels—primary, secondary, tertiary.
– UHC must deliver equity, quality, and continuity of care. - An Agile, Adaptive, and Anticipatory System Is Needed
– Must respond to emergencies (pandemics, climate-related disasters).
– Should integrate traditional medicine, allopathy, and preventive services.
– Must anticipate demographic, environmental, and economic transitions. - Strengthening Primary Healthcare Is Critical
– Frontline care must be robust, accessible, and community-centred.
– Supply chains for diagnostics, vaccines, and medicines must be reliable. - Gender Equity in Health Access
– Women’s lower healthy life expectancy (HLE) compared to men underscores inequity.
– Maternal mortality, NCDs in women, and mental health disparities need urgent attention. - Education and Intergenerational Health Links
– Improved education enables better nutrition, sanitation practices, and health awareness.
– School-based health promotion should be strengthened. - Climate Change and Environmental Risks
– Floods, zoonotic outbreaks, heatwaves, pollution, and antimicrobial resistance threaten health systems.
– India must prepare for rising climate-linked diseases and environmental degradation. - Financing and Universal Health Assurance
– UHC requires predictable and adequate financing.
– Public and private sectors must be integrated without diluting public accountability. - Strengthening Community Participation
– Health systems must involve communities in decision-making and local health planning.
III. AUTHOR’S STANCE AND POSSIBLE BIASES
- Strongly Public Health-Oriented Viewpoint
– The author emphasises strengthening public systems over market-driven models. - Optimistic but Normative Position
– The roadmap is aspirational; implementation challenges are acknowledged but not deeply analysed. - Limited Critique of Existing Government Schemes
– Schemes like Ayushman Bharat and Health & Wellness Centres are mentioned but not scrutinised for gaps, budget shortfalls, or uneven performance across states. - Underplays the Role of Private Healthcare
– India’s mixed health system reality—where private providers serve a majority—is treated cautiously but without a deep integration roadmap. - Focus on Systemic Preparedness More Than Fiscal Reality
– The fiscal constraints and political economy challenges of UHC are understated.
IV. PROS OF THE ARTICLE (Strengths)
1. Holistic and Forward-Looking Vision
– Combines health service delivery, workforce readiness, climate adaptation, gender equity, and community participation.
2. Strong Emphasis on Primary Health Systems
– Correctly identifies primary healthcare as the backbone of UHC.
3. Integrates Climate, Demography, and Epidemiology
– Acknowledges emerging threats (zoonotic diseases, AMR, environmental degradation).
4. Highlights Gender and Social Inequities
– Recognises disparities in HLE, access, and outcomes.
5. Advocates Preventive and Promotive Care
– Recognises that UHC must go beyond curative treatment.
6. Focus on Workforce Mobilisation and Resilience
– Pandemic lessons on rapid workforce deployment are well-integrated.
V. CONS OF THE ARTICLE (Limitations & Critical Gaps)
1. Lacks Discussion on Funding Feasibility
– UHC requires significant increases in public health spending (currently ~2% of GDP).
– The article does not outline how to overcome fiscal constraints.
2. Understates Nationwide Health Inequality
– Vast disparities between states (Kerala vs Bihar) and urban vs rural remain underexplored.
3. Missing Detailed Strategy for Private Sector Regulation
– A mixed healthcare system requires stronger regulatory frameworks—largely unaddressed here.
4. Limited Attention to Technology Integration
– Digital health, telemedicine, and Ayushman Bharat Digital Mission are not given sufficient focus.
5. Human Resources Challenges Underexplored
– India faces severe shortages of specialists, nurses, and allied workers; recruitment and retention issues need deeper analysis.
6. No Mention of Insurance Design Limitations
– Insurance-heavy models often neglect outpatient care and primary care—critical for UHC.
7. Fragility of Supply Chains Not Fully Addressed
– The pandemic exposed weaknesses that require systemic overhaul.
VI. POLICY IMPLICATIONS (UPSC GS-II & GS-III Relevance)
- Legal Framework for UHC
– Constitutional or legislative backing for the right to health.
– Institutionalisation of essential health service guarantees. - Strengthening Primary Healthcare
– Expansion of Health & Wellness Centres.
– More investment in ASHAs, ANMs, and PHCs. - Financing Reform
– Increase public health expenditure to 2.5–3% of GDP.
– Move from insurance-based to primary care-oriented financing models. - Human Resources for Health
– Improve workforce training, retention, and career progression.
– Emergency mobilisation frameworks. - Regulating Private Sector
– Transparent pricing, standard treatment guidelines, patient rights, and grievance systems. - Addressing Gender and Social Inequities
– Targeted programmes for maternal health, NCDs in women, and vulnerable groups. - Climate-Responsive Health Planning
– Early warning systems, heat preparedness, zoonotic disease surveillance. - Community Participation and Decentralised Governance
– Empower Panchayati Raj institutions and urban local bodies in health planning.
VII. REAL-WORLD IMPACT ASSESSMENT
- Reduction in Catastrophic Health Expenditure
– UHC can prevent millions from falling into poverty due to medical costs. - Improved Health Outcomes
– Control of NCDs, reduction in maternal and infant mortality. - Stronger Pandemic Preparedness
– Agile and anticipatory health systems can rapidly scale emergency responses. - Equity and Social Justice
– Better access for women, rural communities, and marginalised groups. - Economic Growth
– A healthier workforce boosts productivity and national development. - Challenges Remain Significant
– Financing, governance, and political will are major constraints.
VIII. BALANCED CONCLUSION
The article offers a comprehensive and visionary roadmap for Universal Health Coverage, emphasising preparedness, adaptability, and inclusivity. It rightly foregrounds primary care, gender equity, climate resilience, and community engagement—crucial components for a functional and equitable health system.
However, a more grounded analysis of fiscal realities, private sector integration, inter-state disparities, and governance challenges would strengthen the roadmap. UHC is as much a political and administrative challenge as a technical one. Achieving it demands sustained investment, coalition-building, and systemic reform.
IX. FUTURE PERSPECTIVES (UPSC Mains-Ready Insights)
- Enact a National Health Act guaranteeing essential services.
- Strengthen public health infrastructure, especially in underserved regions.
- Expand digital health innovations to improve access and efficiency.
- Implement workforce reforms, including fair wages and training.
- Increase fiscal space through health taxes, rationalised subsidies, and strategic purchasing.
- Build climate-adaptive, resilient health systems.
- Promote public-private partnerships with strong accountability frameworks.
- Integrate health in all sectors—urban planning, education, environment, and transport.
With political will, financial commitment, and robust governance, India can move steadily toward a universal, equitable, and resilient health system.
